Ventilators have received a lot of attention in the news lately. Why are they so important? A ventilator (vent) is a

machine that can breathe for a person when her lungs are not functioning properly. The vent will help the patient ventilate (eliminate carbon dioxide) and oxygenate until the issue that is causing the lungs problem(s) resolves. In addition, since a ventilator can take over the work of breathing for a patient, it means that the patient will expend less energy when being supported by a vent, which means the patient will be consuming less oxygen and will thus be conserving precious oxygen for the body’s other demands.
In short, a ventilator can help a patient maintain adequate oxygenation and ventilation, and it can help the body rest and conserve oxygen. A vent can “take over” until the lungs heal and the underlying illness has resolved.
When a patient needs to be placed on a vent, the medical team will put a breathing tube down through the patient’s mouth and into the upper airway. This is called intubation. This breathing tube (endotracheal (ET) tube) will be connected to tubing that goes to a vent. The patient is now “intubated” and receiving “mechanical ventilation,” which means the vent is doing all or some of the breathing for the patient. In many cases of respiratory failure, the vent will be doing all of the breathing for the patient early on.
An ET tube helps keep an airway patent or open. This is important if it is thought that a patient’s airway is “swelling,” which can occur with smoke inhalation. Swelling may also occur after neck surgery when there is internal bleeding near the airway, which can essentially push the airway closed.
Further, an ET tube makes it easier to suction a patient, which is important when patients have conditions such as acute respiratory distress syndrome (ARDS).
As a patient gets better, the vent will be set to do less and less breathing for her, until she is sufficiently weaned and passes certain tests that show she can breathe on her own and clear her own secretions. Then, the ET tube will be removed.
WHAT IS ARDS?
People are talking a lot about ARDS and viral infection, and most of these patients need a ventilator. The reason there is a ventilator shortage is because so many people currently have ARDS and need ventilatory support.
The lungs are made up of millions of tiny sacs called alveoli. One of the critical functions of the alveoli is the absorption of oxygen into the blood stream, which carries oxygen to all the cells (and organs) in the body. Another critical function is the elimination of carbon dioxide, which is an end product of cellular metabolism. Too much carbon dioxide in the body causes a low pH, or acidosis.
In ARDS, the patient has widespread damage to the alveoli and to the capillaries (tiny blood vessels) that surround
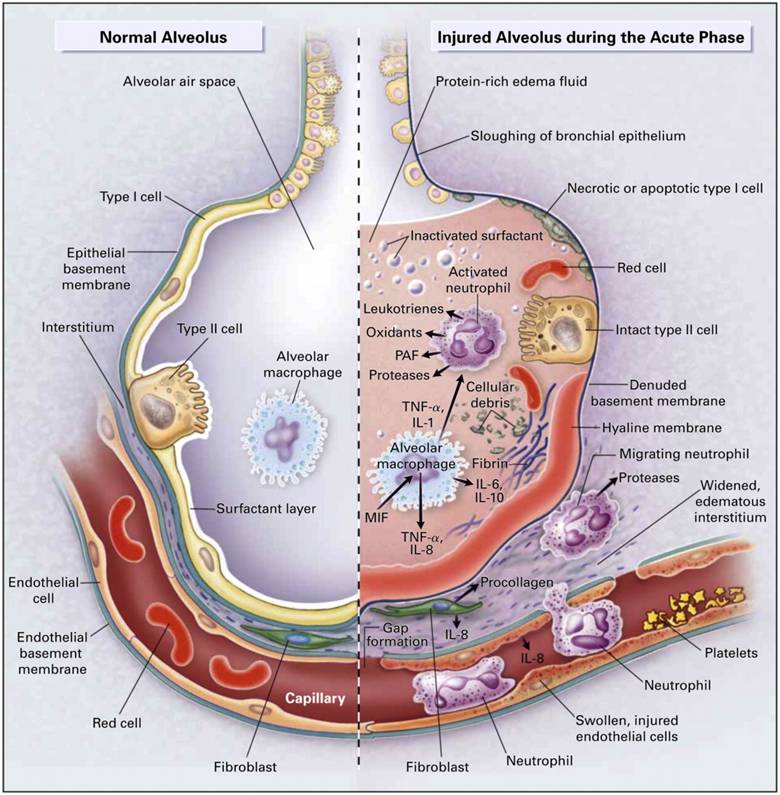
the alveoli. In other words, there is widespread damage to the alveolar capillary bed. The alveolar capillary bed is where gas exchange (i.e., oxygen and carbon dioxide exchange) takes place via gases diffusing between the capillaries and alveoli. Damage to the alveolar capillary bed results in the tissue around the alveoli and the alveoli itself filling with fluid (called pulmonary edema). Patients with ARDS have pink, frothy secretions because their lungs are filled with fluid that contains blood, protein and debris from degenerating cells.
Patients with ARDS typically have a lot of fluid in their lungs as well as stiff lungs.
When the aforementioned damage to the lungs occurs and fluid builds up, there is a lot of alveolar collapse (“lung collapse”).
Here is a list of the potential consequences of ARDS:
IMPAIRED GAS EXCHANGE
With ARDS, there is less oxygen going into the blood stream, depriving organs of the normal amount of oxygen. In addition, there is less elimination of carbon dioxide, which can cause the patient to have increased acidity in the blood and tissues. In short, ARDS patients often become deprived of sufficient oxygen, and they may also become acidotic. A severe lack of oxygen, called severe hypoxia, can lead to cardiopulmonary arrest. The healthcare team will take measures to prevent hypoxia, and they may even give additional therapies, such as extracorporeal membrane oxygenation (ECMO), which is a machine that can totally bypass the lungs: a patient’s blood is circulated out of the body and into a machine, which removes carbon dioxide and adds oxygen to the blood. ECMO is only rarely used.
-
THE LUNGS BECOME STIFF
When the lungs become stiff, it is very hard for a patient to be properly ventilated with the vent. With ARDS, the lungs become stiff because the condition causes the lungs to not be properly aerated. Even small volumes of air being delivered by the vent can cause very high increases in lung pressures, which can cause further damage to the lungs. The respiratory team will pay very close attention to the lung pressures and will adjust the vent accordingly.
-
PULMONARY HYPERTENSION (PH)
PH occurs in about 25% or people who have ARDS, and it can sometimes (rarely) cause enlargement of the right side of the heart and right sided heart failure.
TREATMENT OF ARDS
Treatment of ARDS is largely supportive, which means the medical team will do everything they can to help promote adequate oxygenation and perfusion (blood flow to the organs), and to keep the body healthy.
In addition to supportive care, ARDS treatment requires management of hypoxemia (insufficient oxygen in the blood), which leads to hypoxia (insufficient oxygen in the tissues / organs). Treatment also requires the management and prevention of acidosis.
Supportive Care
Patients with ARDS require a lot of supportive care, including use of sedatives and neuromuscular blocks to minimize oxygen consumption and to prevent the patient from fighting the vent. In addition, patients need good hemodynamic management, nutritional support, control of blood sugar, expeditious evaluation and treatment of hospital-acquired pneumonia, and prophylaxis against blood clots and gastrointestinal bleeding.
Management of Hypoxemia
As discussed, many people with ARDS will require intubation and mechanical ventilation.

- The healthcare team will use lung protective strategies and prevent pressures in the lungs from being too high.
- The team will use the lowest amount of oxygen possible to prevent lung damage caused by toxic oxygen species.
- The team will use low tidal volumes (volume of air delivered by the vent per breath) and PEEP (positive end expiratory pressure), and will closely monitor the patient’s response to the vent settings, including lung pressures.
In short, ARDS requires very close monitoring of the vent and the patient’s response to the vent setting, so the pulmonary and respiratory therapy teams may be in patients’ rooms quite frequently.
NEWS FROM PHYSICIANS AND RESPIRATORY THERAPISTS
What we are hearing from Detroit-based physicians and respiratory therapists is that some people with ARDS have been able to be weaned off their ventilators pretty quickly and are now doing very well.
However, some patients with the virus and ARDS may need to be on a ventilator for several days or even weeks.
TREATMENTS TO PREVENT / REDUCE THE SEVERITY OF ARDS
To help slow down or halt a cytokine storm (which is a major component in the development of ARDS), physicians are giving tocilizimab (IL-6 cytokine), which at this point is a theoretical treatment. Physicians are also using Remdesivir, which is a drug that has been found to have antiviral activity against coronaviruses. In addition, solumedrol is given when a patient receives a diagnosis of ARDS.
Our heart goes out to the many people who have been hospitalized, and we applaud all the healthcare workers who are risking their lives to help these patients.
Scott Weidenfeller is a trial lawyer who has been named a Super Lawyer every year for the last decade. He is an executive board member of the Michigan Association for Justice, and has received certificates of appreciation for his federal pro bono work.
Prior to attending law school and working for Grewal Law, Alison Taylor worked as a respiratory therapist and was involved in ECMO and liquid lung ventilation research.
SOURCES AND ADDITIONAL READING
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2763184?appId=scweb
https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19
https://www.newscientist.com/term/cytokine-storm/
https://jintensivecare.biomedcentral.com/articles/10.1186/s40560-018-0321-9
https://www.drugtopics.com/latest/phase-3-trial-evaluate-tocilizumab-severe-covid-19-pneumonia
https://www.cdc.gov/coronavirus/2019-ncov/hcp/therapeutic-options.html
Artigas A, Bernard GR, Carlet J, et al. The American-European Consensus Conference on ARDS, part 2: Ventilatory, pharmacologic, supportive therapy, study design strategies, and issues related to recovery and remodeling. Acute respiratory distress syndrome. Am J Respir Crit Care Med 1998; 157:1332.
ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA 2012; 307:2526.
Rubenfeld GD, Caldwell E, Peabody E, et al. Incidence and outcomes of acute lung injury. N Engl J Med 2005; 353:1685.
World Health Organization. Director-General’s remarks at the media briefing on 2019-nCoV on 11 February 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020.
Centers for Disease Control and Prevention. 2019 Novel coronavirus, Wuhan, China. Information for Healthcare Professionals. https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html.
World Health Organization. Novel coronavirus situation report -2. January 22, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200122-sitrep-2-2019-ncov.pdf.
van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med 2020.
Centers for Disease Control and Prevention. Interim Clinical Guidance for Management of Patients with Confirmed 2019 Novel Coronavirus (2019-nCoV) Infection, Updated February 12, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html.
Lo MK, Jordan R, Arvey A, Sudhamsu J, Shrivastava-Ranjan P, Hotard AL, et al. (March 2017). “GS-5734 and its parent nucleoside analog inhibit Filo-, Pneumo-, and Paramyxoviruses”. Scientific Reports. 7 (1): 43395. Bibcode:2017NatSR…743395L. doi:10.1038/srep43395. PMC 5338263. PMID 28262699.
Sheahan TP, Sims AC, Graham RL, Menachery VD, Gralinski LE, Case JB, et al. (June 2017). “Broad-spectrum antiviral GS-5734 inhibits both epidemic and zoonotic coronaviruses”. Science Translational Medicine. 9 (396): eaal3653. doi:10.1126/scitranslmed.aal3653. PMC 5567817. PMID 28659436.
Agostini ML, Andres EL, Sims AC, Graham RL, Sheahan TP, Lu X, et al. (March 2018). “Coronavirus Susceptibility to the Antiviral Remdesivir (GS-5734) Is Mediated by the Viral Polymerase and the Proofreading Exoribonuclease”. mBio. 9 (2). doi:10.1128/mBio.00221-18. PMC 5844999. PMID 29511076.







