Pressure Ulcers and Their Causes
Pressure ulcers, also called pressure sores, bed sores, or decubitus ulcers, are injuries to the skin and underlying tissue caused by prolonged pressure on the skin. According to the Mayo Clinic, they typically develop on skin covering bony areas of the body, such as the heels, tailbone, shoulder blades and hips. People most at risk for pressure ulcers are those who have a condition which confines them to a bed for a long time, or limits their ability to change positions. Prolonged pressure against the skin from a bed (or wheelchair) limits blood flow to the skin and nearby tissues.
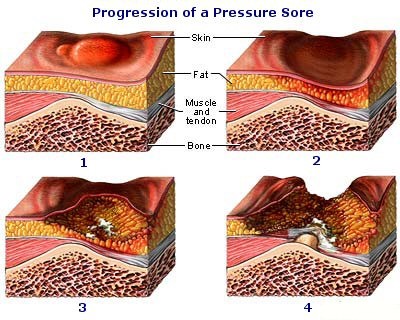
Stages of Pressure Ulcers
Pressure ulcers develop quickly and are very difficult to treat. The National Pressure Ulcer Advisory Panel, an organization dedicated to prevention and treatment of pressure ulcers, has defined stages of pressure ulcer severity. Stage I ulcers show redness and tenderness. Stage IV ulcers involve a large-scale loss of tissue. Stage IV pressure ulcers may expose muscle, bone, or tendons and often extend beyond the wound and into healthy layers of skin. The most severe stage of pressure ulcer is known as “Unstageable,” meaning that there is “full thickness tissue loss in which actual depth is completely obscured by slough and /or eschar in the wound bed.” If allowed to progress, pressure sores can lead to serious and even deadly complications such as cellulitis, sepsis, bone and joint infections, and even squamous cell carcinoma, a type of cancer. Stage III, IV and Unstagable ulcers often require surgical debridement and can take months or even years to heal.
“Never Event”
In 2008, The Center for Medicare and Medicaid Services (CMS) determined that Medicare/Medicaid would no longer cover the extra cost of health care related to the development of a Stage III, IV, or unstageable pressure ulcer while in the course of a hospital admission. Medicare labeled pressure ulcers staged III and above a “Never Event,” meaning “such a shocking medical error it should never occur.” Severe pressure ulcers are among a list of 24 Never Events including: leaving a foreign object or medical instrument in a patient’s body during surgery, patient falls, patient suicide, administration of incompatible blood, surgery on the wrong patient, and injury resulting from certain criminal events in a hospital. Pressure ulcers are costly, with an average charge per stay of $37,800.
When are Pressure Ulcers Unavoidable?
CMS and the Agency for Healthcare Research and Quality have indicated that the risk of Never Events, including pressure ulcers, is significantly influenced by hospital policies and procedures—meaning that if hospitals implement the proper procedures, these events are unlikely to occur. Further, CMS indicated, “Based on the comprehensive assessment of an individual, the facility must ensure that an individual who enters the facility without pressure sores does not develop pressure sores unless the individual’s clinical condition demonstrates that they are unavoidable.”
In 2009, the National Pressure Ulcer Advisory Panel held a conference to discuss avoidability of pressure ulcers. At this conference, clinicians in attendance believed that most pressure ulcers were avoidable. The conference determined that an avoidable pressure ulcer can develop when the provider did not do one or more of the following: evaluate the individual’s clinical condition and risk factors, define and implement interventions consistent with individual needs, individual goals, and recognized standards of practice; monitor and evaluate the impact of interventions; or revise the interventions as appropriate. The conference determined that an unavoidable ulcer occurs only when a provider did all of the above, and an ulcer still developed. Further, turning and/or repositioning the patient every two hours has been common practice and is often considered the standard of care, and medical technology continues to develop products for treatment/avoidance, such as specialty cushions and mattress covers.
As Florence Nightingale, the “mother of nursing” wrote in her notes on nursing, “If he has a bedsore, it’s generally not the fault of the disease, but of the nursing.”
Drawing: Baromedical.ca







